What is HRT? And what’s best for me and my perimenopause?
7 months ago
Perimenopause7 months ago
Perimenopause
Wondering if HRT is right for you? Keen to explore all the options available to you? We chat to Dr Nicky Keay about the science behind the solutions and bust a few myths along the way…
Reviewed by: Dr Nicky Keay.
Sign up to the perimenopause newsletter and waitlist here .
Thanks to Davina McCall’s groundbreaking Channel 4 documentary ‘ Sex, Myths and the Menopause ’, in which the Big Brother presenter talks candidly about how HRT (Hormone Replacement Therapy) helped her manage her hormonal symptoms, more women are shrugging off the HRT stigma and looking at the treatment as a serious option for perimenopause.
As with everything in life, it’s important to know the facts so you can make up your own mind. To help, we asked Dr Nicky Keay , a leading expert in endocrinology, lecturer at UCL and chief medical officer of hormone mapping company Forth to give us the lowdown on the options.
Ok, so in basic terms, it’s the transition time when your main menstrual cycle hormones are declining, but your periods haven’t *quite* finished doing their thing yet. It’s sometimes referred to as the ‘menopausal transition’ and usually starts in your mid 40s (the average age is 47.5), but it can begin as early as your mid-30s or as late as your mid-50s.
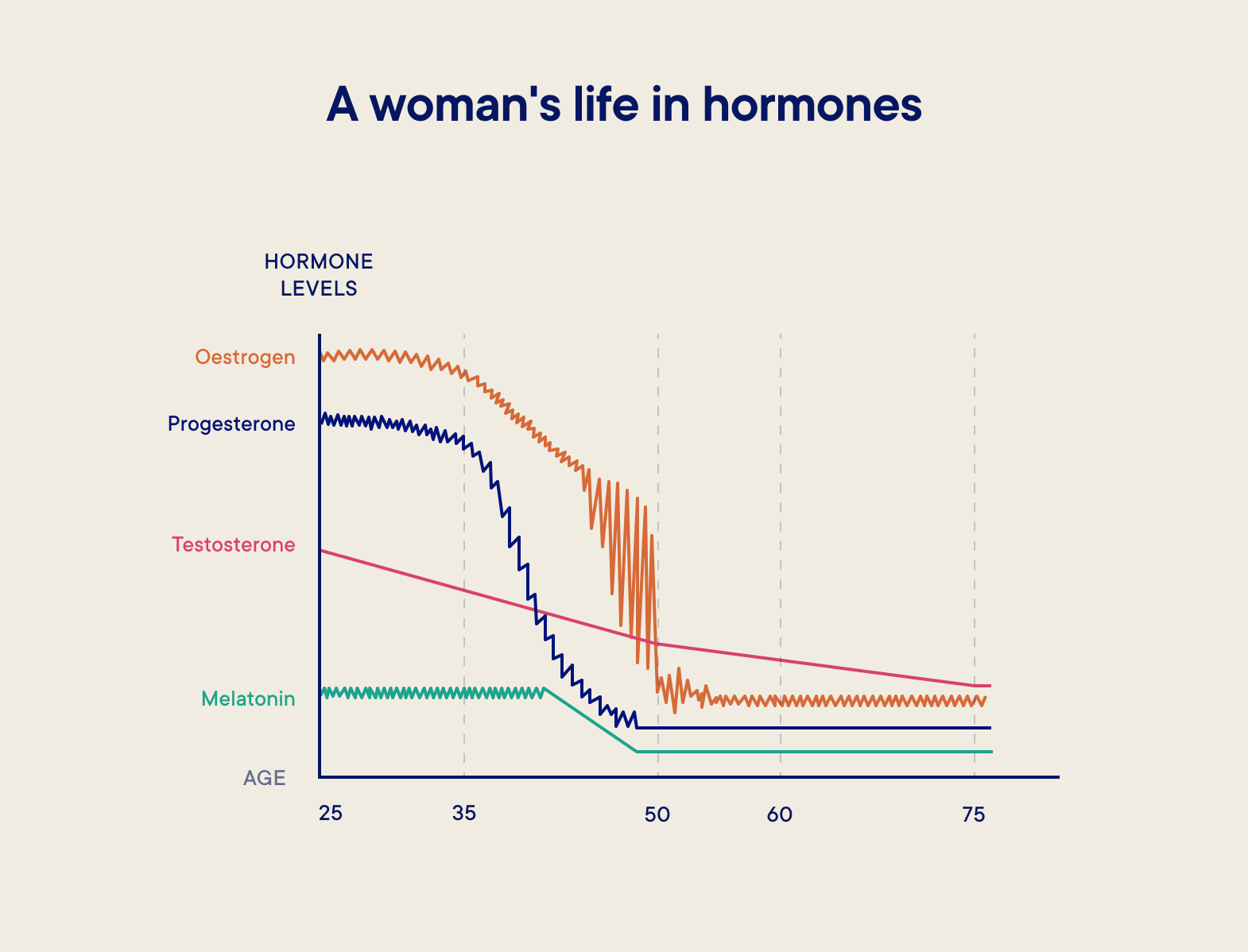
During perimenopause, your oestrogen and progesterone levels naturally start to taper off (while spiking erratically on their way down) and testosterone also declines (see graph below). It’s this that can bring on symptoms like anxiety, mood swings, brain fog, hot flushes and irregular periods.
These symptoms can be tough to manage without the right support, affecting day-to-day comfort and quality of life. In fact, a whopping one in 10 women are reported to have left work because of symptoms of the menopause, so seeking treatment when you need it is pretty vital.
“HRT stands for ‘hormone replacement therapy’,” says Dr Keay. “The treatment replaces some of the hormones in your body to similar levels as they were before the perimenopause started.”
When it comes to HRT, it’s important to know the difference between the NHS-approved ‘body identical hormones’ and so-called ‘bioidentical hormones’. Confusing, we know, as they sound kind of similar.
“Ideally, the HRT you take should utilise body-identical hormones,” says Nicky - these are precise duplicates of human hormones which originate in the human ovary as well as the adrenal and thyroid glands.
Bioidentical hormones, on the other hand, are hormone preparations made from plant sources that some practitioners claim are similar or identical to human hormones. They’re often marketed by private companies as ‘safer’ or ‘more natural’ alternative to NHS-prescribed HRT, but be wary, as they’re unregulated, so it’s unclear how safe or effective they really are.
“Don’t be conned by menopause marketing,” Dr Keay warns. “HRT companies often claim that they have a treatment that you can’t access on the NHS in return for money. That’s not to say that all private practices should be avoided, but I would strongly recommend checking that your doctor is part of the British Menopause Society , as they’ll be up-to-date with the latest research and they won’t be flogging unregulated bioidenticals.”
Body Identical HRT is available on the NHS but, frustratingly, it’s not guaranteed that this will be the first type of HRT that will be offered to you, so you’ll need to specifically ask your GP to ensure that you get it.
What many women don’t realise is that the statistical risk of breast cancer from HRT is exactly the same as taking the contraceptive pill
“Some women look into private companies as they may have previously gone to their GP and been given antidepressants,” says Nicky. “In this case, I would strongly recommend looking at the patient section of the British Menopause Society website and bringing this information along to your GP appointment so that you can steer the conversation towards your HRT options.”
Combined HRT: Most women who go down the HRT route will take a combination of oestrogen and progesterone (known as combined HRT). “You can take oestrogen and progesterone separately or combined in one therapy,” says Keay.
If your GP advises you to take them separately, you may want to take a progesterone tablet with oestrogen patches or gel. Alternatively, an intrauterine device (IUS or coil), such as the Mirena coil, works as a form of progesterone alongside oestrogen tables, patches, gels or sprays.
Oestrogen-only HRT: “Some women will be offered Oestrogen-only HRT by their GP, which is usually only recommended if you’ve had your womb removed during a hysterectomy,” says Nicky. Oestrogen is the heavyweight hormone that helps with the big symptoms like hot flashes and vaginal dryness, and, as an added bonus, it strengthens your bones too, lowering your risk of osteoporosis.
HRT comes in several different forms, which your GP can talk you through.
Tablets: Both Oestrogen-only and combined HRT are available as tablets, which you take once per day. Lots of women choose this option as it’s easy to take on-the-go, although some of the risks of HRT, such as blood clots, are higher with tablets than with other forms.
Skin patches: This option involves sticking a self-adhesive patch on your skin below your waist, which transdermally releases hormones into the body through your skin. You remove the patch and repapply a new one every week, choosing a different area of skin each time. “The safest and best form of HRT is taking Oestrogen through the skin,” stresses Dr Keay, although she believes patches can have drawbacks as you can’t alter the dose.
Gels: Once you’ve applied HRT gel to a clean area of skin, such as the shoulder or arm, you allow it to dry for five minutes and then wash your hands thoroughly. “It’s personal preference but I think that the gel is really great,” says Dr Keay. “It comes in small sachets like energy gels and there are different sizes, so you can really fine tune it to what you need.”
Sprays: Oestrogen-only HRT is available as a body spray too, that you spray onto dry skin - usually on the forearm or inner thigh. The absorption of sprays, gels and patches is more reliable than taking HRT as a tablet because it goes straight into your bloodstream through your skin.
Implants: Oestrogen-only implants are much less common. The small implants are inserted under the skin and release oestrogen gradually. As they last for several months, they can be convenient if you struggle with remembering to take medication on the regular. Word to the wise though: if you haven’t undergone a hysterectomy, you'll need to take progestogen separately too.
Let’s face it, HRT has had a bad rep over the past few decades, but as Davina McCall’s documentary highlights, the benefits massively outweigh the risks for many women.
Research that did the rounds in the media in the ’90s suggested that HRT had a high breast cancer risk, but it later emerged that the study was flawed in its execution and interpretation. Since then, fresh research has proved the HRT benefits, changing our view on the cancer connection.
The NICE guidelines state that for women around menopausal age, oestrogen-only HRT causes little or no change in the risk of breast cancer. That said, HRT that contains oestrogen and progesterone may increase your breast cancer risk, and this risk may be higher if you take HRT for longer. The good news? It also falls again when you stop taking HRT.
No matter which route you decide to go down, lifestyle interventions, such as staying healthy, moving more and taking time out for you will certainly complement the choice you make
HRT tablets (but not patches or gels) are also linked with a higher risk of developing blood clots too. If you’re already at higher risk of blood clots and you’re considering HRT, you’ll likely be offered patches or gel rather than tablets.
If you start HRT before you're 60, it doesn’t increase your risk of cardiovascular disease, and there’s no evidence to suggest that it increases your risk of dementia or type 2 Diabetes either.
“It’s a real tragedy that there is so much misinformation about HRT,” says Nicky. “What many women don’t realise is that the statistical risk of breast cancer from HRT is exactly the same as taking the contraceptive pill. Of course, we should be absolutely open and frank about the negatives, but we should highlight the positives too.”
If you don’t fancy going down the HRT route, or your GP has advised against it, there are lots of herbal remedies that claim to treat menopausal symptoms such as hot flushes.
Evening primrose oil, black cohosh, angelica, ginseng and St John's wort are just some of the herbal products you’ll find people promoting as effective solutions for perimenopausal symptoms. Unfortunately, there’s limited evidence that herbal remedies work, and because they aren’t prescribed by a GP, the quality, purity and dose can wildly differ.
“I don’t like advising people to take St John’s wort in particular, as it can interfere with other medications, so it’s really important to chat to your GP if you’re thinking about using a complementary therapy,” says Dr Keay.
Although the Davina documentary has opened up conversations about HRT, not everyone wants it, not everyone needs it and not everyone can have it. For these women, there are loads of other options available.
Cognitive Behavioural Therapy (CBT) can be a really useful tool for tackling the low mood and anxiety that can arise as a result of the menopause. The talking therapy, which helps you to reframe negative thoughts, can also have a positive effect on hot flushes too, as research has found that anticipating a hot flush can increase its severity and duration. And if you’re struggling to get a decent night’s kip, the psychological treatment can also help to reduce stress, having a beneficial effect on sleep.
Yoga and breathing exercises have been linked to improved sleep quality and reduced psychological symptoms in both peri and menopausal women. And acupuncture is another non-hormonal perimenopause option.
A 2019 study found that five weeks of the traditional Chinese medicine (in which thin needles are inserted into the body) reduced hot flashes, night sweats, mood swings, and sleep disruptions in women dealing with menopause symptoms, although researchers couldn’t *exactly* rule out a placebo effect.
Regardless of whether you go down the HRT or non-hormonal therapy route, adopting or maintaining healthy lifestyle habits can positively help your symptoms.
Exercise is a proven intervention for easing some perimenopause symptoms, with particular emphasis on strength and resistance training for bone health, metabolism and muscle maintenance (find out more about perimenopause fitness here ). But eating well and limiting things that contribute to anxiety, hot flushes or poor sleep, such as caffeine and alcohol, can also help.
“When it comes to HRT, it all comes down to the quality of a woman’s life and the choice of the individual,” says Dr Keay. “I take HRT myself and I am a big advocate for its benefits for those that are eligible to take it too,” she says, but adds that talking therapies, meditation and other complementary treatments that lower stress and anxiety can be very effective, too.
No matter which route you decide to go down, lifestyle interventions, such as staying healthy, moving more and taking time out for you will certainly complement the choice you make.
For anyone looking for further advice on HRT, Dr Keay says that The British Menopause Society website is a great tool for finding a local specialist who is a current member of the BMS and has demonstrated specialist competency in menopause.
 Cycle syncing
Cycle syncing Perimenopause
Perimenopause Perimenopause
Perimenopause Perimenopause
PerimenopauseSign up to learn everything you need to know about CycleMapping, plus how you can live better and feel better through optimising your fitness to you.
This website uses cookies to ensure you get the best experience on our website. Learn more

Sign up for the very latest news on women's fitness, health and hormones, plus be the first to receive exclusive offers and extras